Important Safety Information
CONTRAINDICATIONS
- Hypersensitivity to gonadotropin-releasing hormone (GnRH), GnRH agonists, or any of the excipients in LUPRON DEPOT-PED.
Anaphylactic reactions to synthetic GnRH or GnRH agonists have been reported.
- Pregnancy: LUPRON DEPOT-PED may cause fetal harm.
WARNINGS AND PRECAUTIONS
Initial Rise of Gonadotropins and Sex Steroid Levels
- During the early phase of therapy or after subsequent doses, gonadotropins and sex steroids may rise above baseline because of the initial stimulatory effect of the drug. Therefore, an increase in clinical signs and symptoms of puberty, including vaginal bleeding, may be observed during the first weeks of therapy or after subsequent doses.
Psychiatric Events
- Psychiatric events have been reported in patients taking GnRH agonists, including LUPRON DEPOT-PED. Postmarketing reports with this class of drugs include symptoms of emotional lability, such as crying, irritability, impatience, anger, and aggression. Monitor for development or worsening of psychiatric symptoms during treatment.
Convulsions
- Postmarketing reports of convulsions have been observed in patients receiving GnRH agonists, including LUPRON DEPOT-PED. These included patients with a history of seizures, epilepsy, cerebrovascular disorders, central nervous system anomalies or tumors, and patients on concomitant medications that have been associated with convulsions, such as bupropion and SSRIs. Convulsions have also been reported in patients in the absence of any of the conditions mentioned above.
Pseudotumor Cerebri (Idiopathic Intracranial Hypertension)
- Pseudotumor cerebri (idiopathic intracranial hypertension) have been reported in pediatric patients receiving GnRH agonists, including LUPRON DEPOT-PED. Monitor patients for signs and symptoms of pseudotumor cerebri, including headache, papilledema, blurred vision, diplopia, loss of vision, pain behind the eye or pain with eye movement, tinnitus, dizziness, and nausea.
ADVERSE REACTIONS
- The most common (≥2%) adverse reactions in clinical studies with LUPRON DEPOT-PED 7.5 mg, 11.25 mg, and 15 mg for 1-month administration were: injection site reactions including abscess, emotional lability, acne/seborrhea, vaginitis/vaginal bleeding/vaginal discharge, pain, rash including erythema multiforme, headache, and vasodilation.
- The most common (≥2%) adverse reactions in clinical studies with LUPRON DEPOT-PED 11.25 mg and 30 mg for 3-month administration were: injection site pain, increased weight, headache, altered mood, and injection site swelling.
- The most common (≥4%) adverse reactions in clinical studies with LUPRON DEPOT-PED 45 mg for 6-month administration were: injection site reactions, headache, psychiatric events, abdominal pain, diarrhea, hemorrhage, nausea and vomiting, pyrexia, pruritus, pain in extremities, rash, back pain, ligament sprain, increased weight, fracture, breast tenderness, insomnia, chest pain, and hyperhidrosis.
- Diagnostic tests of pituitary gonadotropic and gonadal functions conducted during treatment and up to 6 months after discontinuation may be affected.
- The safety and effectiveness of LUPRON DEPOT-PED have not been established in pediatric patients less than 1 year old.
- LUPRON DEPOT-PED must be administered by a healthcare professional.
Please click here for full Prescribing Information, or visit www.rxabbvie.com/pdf/lupronpediatric.pdf
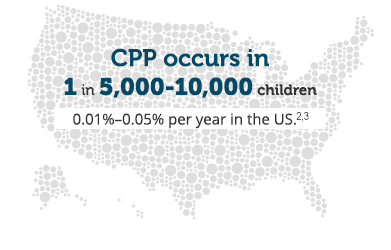
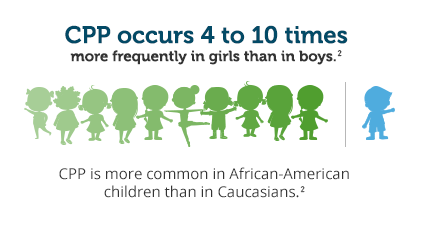
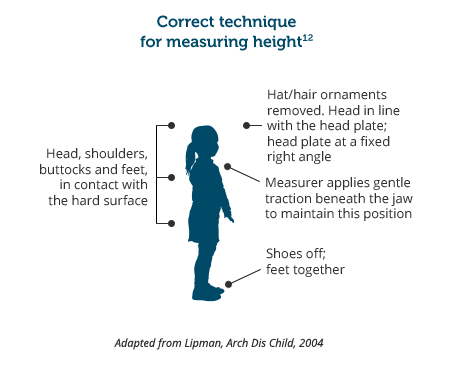
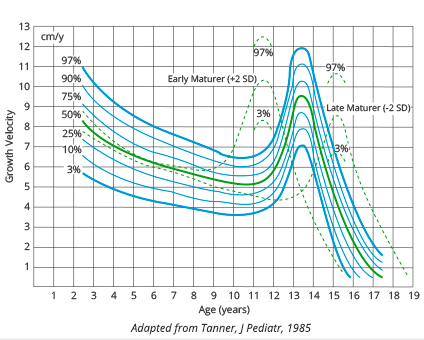
References: 1. Nebesio TD, Eugster EA. Current concepts in normal and abnormal puberty. Curr Probl Pediatr Adolesc Health Care. 2007;37(2):50-72. 2. Muir A. Precocious puberty. Pediatr Rev. 2006;27(10):373-381. 3. González ER. For puberty that comes too soon, new treatment highly effective. JAMA. 1982;248(10):1149-1151. 4. Imel EA, Bethin KE. Etiology of gonadotropin-dependent precocious puberty. In: Pescovitz OH, Walvoord EC, eds. When Puberty Is Precocious: Scientific and Clinical Aspects. Totowa, NJ: Humana Press; 2007:chap 15. 5. Pediatric Endocrine Society/American Academy of Pediatrics Section on Endocrinology Patient Education Committee. Precocious puberty: a guide for families. June 17, 2020. Accessed March 30, 2023. https://pedsendo.org/wp-content/uploads/2020/06/E-Precocious-Puberty.pdf. 6. Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44(235):291-303. 7. Marshall WA, Tanner JM. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970;45(239):13-23. 8. Kaplowitz PB. Precocious puberty. Medscape website. Updated January 24, 2022. Accessed March 30, 2023. https://emedicine.medscape.com/article/924002-overview. 9. Blondell RD, Foster MB, Dave KC. Disorders of puberty. Am Fam Physician. 1999;60(1):209-218. 10. Cooke DW, Divall SA, Radovick S. Normal and aberrant growth. In: Melmed S, Polonsky KS, Larsen PR, Kronenberg HM, eds. Williams Textbook of Endocrinology. 12th ed. Philadelphia, PA: Elsevier Saunders; 2011:chap 24. 11. Tanner JM, Davies PSW. Clinical longitudinal standards for height and velocity for North American children. J Pediatr. 1985;107(3):317‐329. 12. Lipman TH, Hench KD, Benyi T, et al. A multicentre randomised controlled trial of an intervention to improve the accuracy of linear growth measurements. Arch Dis Child. 2004;89(4):342-346. 13. Herman-Giddens ME. Puberty is starting earlier in the 21st century. In: Pescovitz OH, Walvoord EC, eds. When Puberty Is Precocious: Scientific and Clinical Aspects. Totowa, NJ: Humana Press; 2007:chap 5. 14. Brown RT. Adolescent growth and development. In: Holland-Hall C, Brown RT, eds. Adolescent Medicine Secrets. Philadelphia, PA: Hanley & Belfus; 2002:21-28. 15. Carel JC, Lahlou N, Roger M, Chaussain JL. Precocious puberty and statural growth. Hum Reprod Update. 2004;10(2):135-147. 16. Nabhan ZM, Walvoord EC. Treatment of gonadotropin-dependent precocious puberty. In: Pescovitz OH, Walvoord EC, eds. When Puberty Is Precocious: Scientific and Clinical Aspects. Totowa, NJ. Humana Press; 2007:345-362. 17. Carel JC, Eugster EA, Rogol A, et al. Consensus statement on the use of gonadotropin-releasing hormone analogs in children. Pediatrics. 2009;123(4):e752-e762. 18. LUPRON DEPOT-PED [package insert]. North Chicago, IL: AbbVie Inc. 19. Neely EK, Lee PA, Bloch CA, et al. Leuprolide acetate 1-month depot for central precocious puberty: hormonal suppression and recovery. Int J Pediatr Endocrinol. 2010;2010:398639. doi:10.1155/2010/398639.